Explore
Types
Categories
- Nature
- Forest
- Plants
- Space
- Anime
- Animals
- Deer
- Panda
- Rabbit
- Lizard
- Jellyfish
- Goldfish
- Birds
- Eagle
- Flamingo
- Technology
- Cool
- Love
- Valentine's
- Flowers
- Sunflower
- Cars
- Fruit
- Lemon
- Food
- Chocolate
- Art
- Vintage
- Geometric
- Fantasy
- Vampire
- Werewolf
- Happy
- Holi
- Easter
- Inspirational
- Time
- Sports
- Baseball
- People
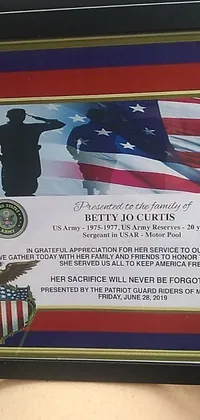
- Army
- Auto
- Trucks
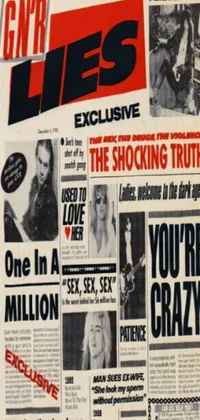
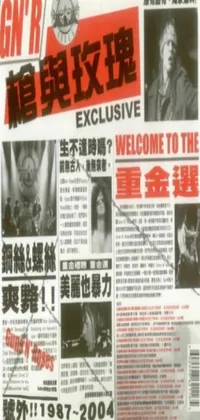
- Music
- Insects
- Ladybug
- Caterpillar
- Cities
- Travel
- Weapons
- All Categories
Color